We’ve covered Arkansas’s rural health care crisis pretty extensively at For AR People. If you’re just now hearing of it, the crisis is so bad that it threatens the survival of hospitals and the well-being of pregnant women across the state.
A new report from the Center for Healthcare Quality and Payment Reform reveals that 30 of Arkansas’s 47 rural hospitals are at risk of closing within the next six to seven years, with 11 at immediate risk.1 It’s essential to remember these closures aren’t just numbers on a spreadsheet. They represent life-threatening gaps in access to care for tens of thousands of Arkansans. They represent people who will go without care.
Most of these hospitals are losing money on the care they provide, especially when it comes to patients who are uninsured or rely on Medicaid. In fact, 79% of Arkansas rural hospitals operated at a loss on patient services last year. As federal COVID-era relief dries up and a new federal budget bill cuts Medicaid spending in rural areas by an estimated $155 billion over the next decade, the outlook grows more grim.
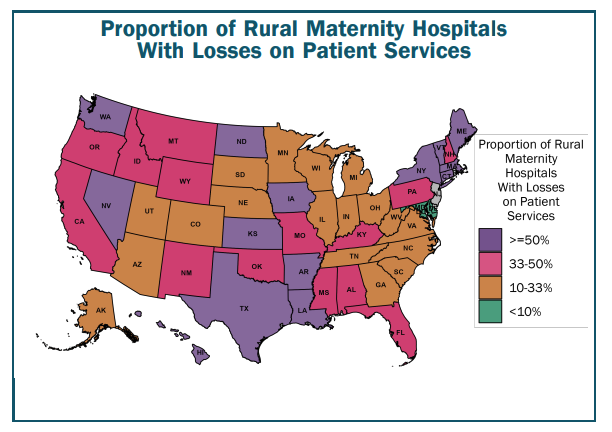
In rural southwest Arkansas, the impact is already felt. Labor and delivery units have vanished from towns like Arkadelphia and Texarkana. Only 33 hospitals in 22 of Arkansas’s 75 counties still offer labor and delivery services, 2 which is a truly staggering statistic. Expecting moms have to drive hours for basic prenatal care, if they can afford the gas money.
That’s why mobile clinics like AR MOMS are stepping in to fill the gap. The federally funded program currently operates in eight towns and serves 11 counties in southwest Arkansas, offering check-ups, mental health care, and help accessing housing or transportation assistance.
But the stopgap may not last because the mobile clinics are funded by a federal grant set to expire next year — a clear link between policy and its impact on everyday people. The clinic’s director believes the mobile initiative can stretch remaining funds but worries about scaling back services if federal support isn’t renewed.
The recently passed Healthy Moms, Healthy Babies Act may provides a glimmer of hope for rural women’s health care. The bipartisan legislation increased Medicaid reimbursement rates for obstetric care and allowed billing for doulas and perinatal mental health providers. This shift will be essential in towns where the vast majority of patients are on Medicaid and where hospital reimbursements are chronically low.
But reimbursement from private insurance, not just Medicaid, remains the single largest source of financial loss for rural hospitals, according to the Democrat Gazette. Without comprehensive reform, hospitals will continue to struggle, and patients like expecting moms will continue to bear the consequences. We need much more than a glimmer of hope to fix the problem.